Financial News
More News
View More
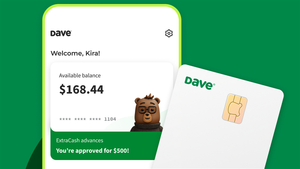
Dave Stock: 180% Gain + Q3 Beat = Breakout Setup?
Today 14:27 EST
Cameco Stock Falls After Earnings, Why the Dip May Be a Gift
Today 13:03 EST
Amgen Stock: New All-Time Highs Ahead After Earnings Beat
Today 12:18 EST
Netflix Stock Split Explained: What It Means for Investors
Today 11:23 EST
Recent Quotes
View More
Stock Quote API & Stock News API supplied by www.cloudquote.io
Quotes delayed at least 20 minutes.
By accessing this page, you agree to the Privacy Policy and Terms Of Service.
Quotes delayed at least 20 minutes.
By accessing this page, you agree to the Privacy Policy and Terms Of Service.
© 2025 FinancialContent. All rights reserved.